Molly Williams, 62 year old female presents with shortness of breath
The large number of differential diagnoses for shortness of breath can seem overwhelming at first so it is important to apply a structured framework that you can hang your history on. This will hopefully help you tailor your questions to tease out a diagnosis as well as pass exams!
Here we'll divide the diagnoses into the headings: respiratory, cardiology, neurological and 'others'.
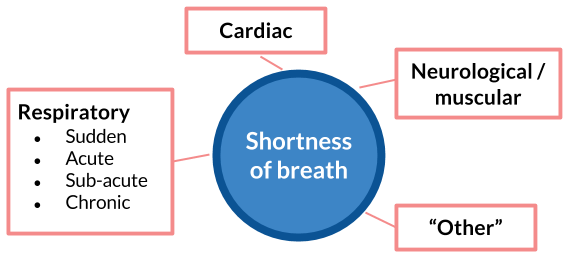
As this is a respiratory case you'll notice we've also included in the list headings for which respiratory diagnoses present in a more acute or chronic setting. This will help you narrow you differentials when taking a history.
Note, not all diagnoses fit neatly under one heading, conditions such as fulminant pulmonary fibrosis can present in days or chronic asthma which can be present for years.
Unsurprisingly, respiratory causes are the most common and most numerous but it is important to keep cardiological causes in mind, particularly in the elderly.
A respiratory history is easier if you focus on just six symptoms:
The answers to these six enquiries should help you narrow down the diagnosis to just a few possibilities.
Remember to still explore the red-flags for cancer and other serious conditions, including the presence of B-symptoms (weight loss, night-sweats etc.) and smoking, pet and occupational history. This is vital not to miss!
Other clues can be found in the patients past medical history (atopy may suggest asthma), drug history (ACE-inhibitors can cause a dry cough), occupational history (exposure to noxious substances), smoking and family history.
Molly Williams is a 62 year old, retired fire-fighter who has become progressively more breathless over the past 3 months, initially only with moderate exercise but now even at rest. In addition she has had a persistent dry cough for the past 1 month. She is otherwise well with no previous respiratory conditions and no smoking history. She has not noticed any weight loss.
Molly has no medical history of note. She has a mild allergy to peanuts and takes no medications other than regular vitamin supplements. Her family history is unremarkable.
Now retired, she was a firefighter in New York for 38 years before moving to the UK last year. She lives in a 2-storey home with her husband and is usually fully independent. She is concerned this may be lung cancer due to her exposure to smoke and dust at work during a time when sufficient safety protection didn't exist.
Go back to the differential list above and have a think; this seems to be due a more insidious cause. If we look at the respiratory causes then lung cancer, COPD and pulmonary fibrosis all fit to some degree with the above history, however, don't ignore potential cardiac problems, particularly in 60+ age group.
Smoking is by far and away the most common cause of COPD and lung cancer in the developed world so her lack of smoking history makes these less likely, however, don't forget about exposure to other particulates such as dust and smoke, particularly given her occupation. In less developed countries, smoke from indoor cooking is a common cause of COPD and cancer.
Finally, remember that pulmonary fibrosis has a multitude of causes including exposure to a number of chemicals, autoimmune causes and idiopathic fibrosis. In respiratory cases knowing the patient's occupation can be a vital clue towards your diagnosis. Mining, farming, construction work and firefighting can all lead to chronic respiratory disease.
Lung cancer is the most common form of cancer in the world and second most in the UK. Despite a decreasing number of cases amongst men, the overall incidence rate has continued to climb over the past 15 years. As medics it is therefore important you understand the underlying processes going on in the lung tissues. The ideas of metaplasia and neoplasia come up again and again in all cancers so try to get used to them!
General inspection: Patient visibly short of breath after talking or moving in bed.
Obs:
Respiratory examination: Molly has mild clubbing in both hands. Chest expansion is reduced bilaterally but percussion is normal over both lung fields. On auscultation there are fine, end-expiratory crackles heard across the whole chest, loudest in the bases.
Cardiac and abdominal examinations: NAD.
Possibly every consultant's favourite question! There are over 20 causes of clubbing but most people get bored if you can recite four, you can start by saying 'the main causes of clubbing fall into either respiratory, cardiac or GI' and then you can give examples:
Spirometry:
| Value | Predicted | % Predicted | |
|---|---|---|---|
| FEV1 | 2.05L | 2.57L | 79.8% |
| FVC | 2.30L | 3.03L | 75.9% |
| FEV1/FVC | 89.1% | 84.8% |
Bloods: FBC and U&Es were normal.
Molly was subsequently sent to hospital for a chest x-ray and further investigation.
Patient treated for ACS.
Wow! You made it all the way to the end. These are the objectives you will have picked up along the way.